Electrochemotherapy (ECT) is a minimally invasive therapy that can be used for the locoregional treatment of spinal metastasis. ECT refers to the concomitant application of reversible electroporation and intravenous administration of bleomycin with ECT enhancing bleomycin uptake into the cells. Electroporation is a phenomenon that occurs when cells are exposed to short, intense electric pulses that induce changes in the transmembrane potential difference. Electroporation requires the insertion of electrodes in or around the tumour followed by the delivery of high-intensity electric pulses to cause cellular membrane damage. Depending on the electric pulse amplitude and the number of pulses applied, electroporation can be reversible, with membrane permeability recovery and cell survival, or irreversible, with loss of cell homeostasis and cell death, termed irreversible electroporation (IRE)1. The purpose of electroporation is to facilitate the passage of non-permeant molecules inside the cell cytoplasm. Bleomycin is the molecule used for ECT because of its capacity to induce mitotic cell death. Indeed, bleomycin binds to DNA and produces single- and double-strand breaks by forming an activated oxygen complex. It is selectively toxic to cells in the M and G2 phases of the cell cycle, and generally more effective against actively dividing rather than resting cells.
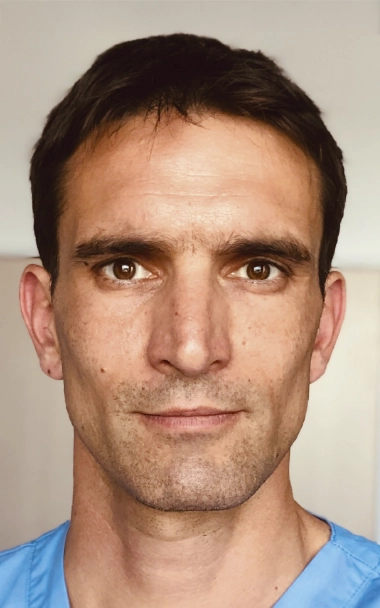
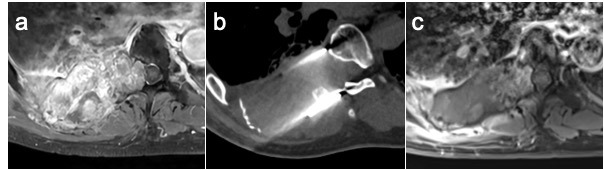
Hence, while IRE may not be ideal for vertebral metastases due to the concern of permanent spinal cord injury, the chemotherapeutic damage caused by RE may provide a novel and unique treatment opportunity. A recent retrospective study2 has demonstrated that ECT could rescue radiotherapy-resistant epidural spinal cord compression in 40 metastatic cancer patients, providing rapid and durable pain relief and neurological improvement. At 1 month, pain was significantly improved over baseline (median Numerical Rating Score: 1.0 [0–8] versus 7.0 [1.0–10], P < .001) and neurological benefits were considered as marked (28%), moderate (28%), stable (38%), or worse (8%). In addition, 1-month post-treatment MRI (35 patients) demonstrated complete response in 46% of patients, partial response in 31%, stable disease in 23%, and no patients with progressive disease.
Based on very promising tumour response rate in bone metastases3, particularly in vertebral metastases2, ECT is becoming a new percutaneous option in the therapeutic arsenal of interventional oncology. It offers an alternative when thermal-ablation techniques are contraindicated and will probably compete with palliative radiotherapy in the near future. However, despite the theoretical safety profile, a 7.5 % occurrence of paraplegia and a 10% occurrence of nerve toxicity have been reported in the literature2 after ECT of spinal metastasis with epidural extension. This toxicity is related to the inevitable inhomogeneity of the electric field between electrodes, with unexpected hyperthermia and IRE at the vicinity of the electrodes’ tips. To enhance ECT’s clinical applicability in the treatment of spinal metastases, further numerical and preclinical studies are required to determine the optimal parameters to create an electric field below the IRE threshold across the spinal cord and over the reversible electroporation threshold across the tumour.